Abstract
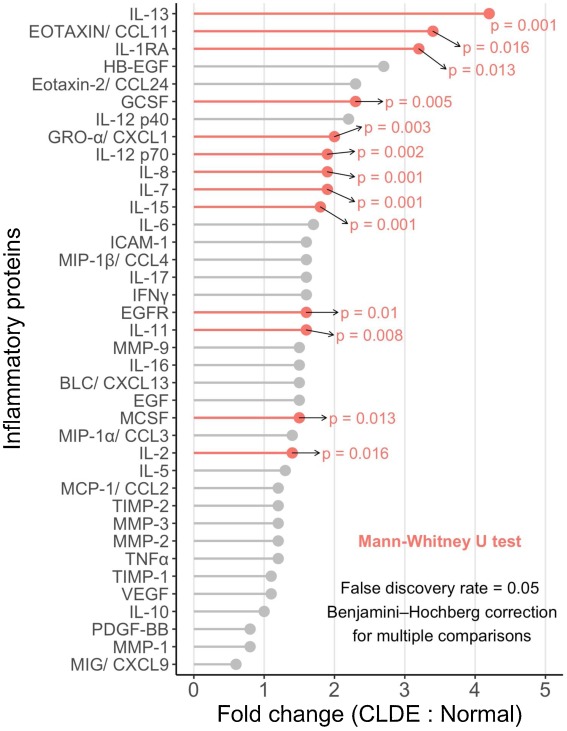
To evaluate the levels and regulation of tear film inflammatory proteins in contact lens-related dry eye (CLDE). One hundred healthy, daily wear (non-overnight), experienced soft contact lens wearers were classified into normal (n = 50) and CLDE (n = 50) groups based on Contact Lens and Dry Eye Questionnaire scores, tear break-up times, and comfort (a two-hour difference between total and comfortable daily lens wear hours). Tear samples (up to 5 μL) were collected by capillary extraction from the inferior meniscus of each eye, and pooled tear samples (10 per group) were tested using a customized Quantibody array. Mann Whitney tests with the Benjamini-Hochberg procedure with a 5% false discovery rate were used to compare the normal and CLDE groups. Relative to the normal group, the CLDE group showed a significantly increased tear concentration of several inflammatory mediators, including interleukin (IL)-7 (p = 0.001), IL-8 (p = 0.001), IL-13 (p = 0.001), IL-15 (p = 0.001), IL-12 p70 (p = 0.002), growth-related oncogene-alpha/ chemokine (C X C motif) ligand 1 (p = 0.003), granulocyte–colony stimulating factor (p = 0.005), IL-11 (p = 0.008), epidermal growth factor receptor (p = 0.01), IL-1 receptor antagonist (RA) (p = 0.013), macrophage colony-stimulating factor (p = 0.013), Eotaxin/C C motif chemokine ligand 11 (CCL11) (p = 0.016), and IL-2 (p = 0.016). The following cytokines were increased three-fold or more in the CLDE group, IL-13 (p = 0.001), Eotaxin/CCL11 (p = 0.016), and IL-1RA (p = 0.013). Several inflammatory markers, including interleukins, were increased in tears of subjects with CLDE. These results support a growing body of evidence that suggests a potential role of inflammation in CLDE.